Post Treatment Lyme Disease (PTLD) represents a research subset of patients who remain significantly ill 6 months or more following standard antibiotic therapy for Lyme disease. PTLD is characterized by a constellation of symptoms that includes severe fatigue, musculoskeletal pain, sleep disturbance, depression, and cognitive problems such as difficulty with short-term memory, speed of thinking, or multi-tasking. In the absence of a direct diagnostic biomarker blood test, PTLD has been difficult to define by physicians, and its existence has been controversial. However, our clinical research shows that meticulous patient evaluation when used alongside appropriate diagnostic testing can reliably identify patients with a history of previously treated Lyme disease who display the typical symptom patterns of PTLD.
Our research indicates the chronic symptom burden related to PTLD is significant. Although often invisible to others, the negative impact on quality of life and daily functioning is substantial for PTLD sufferers.
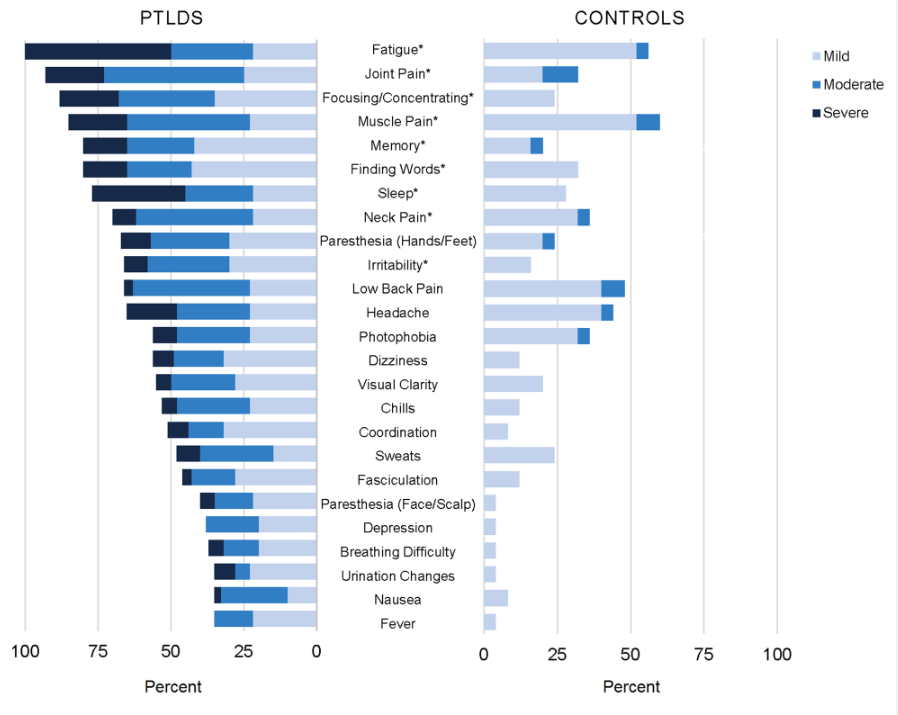
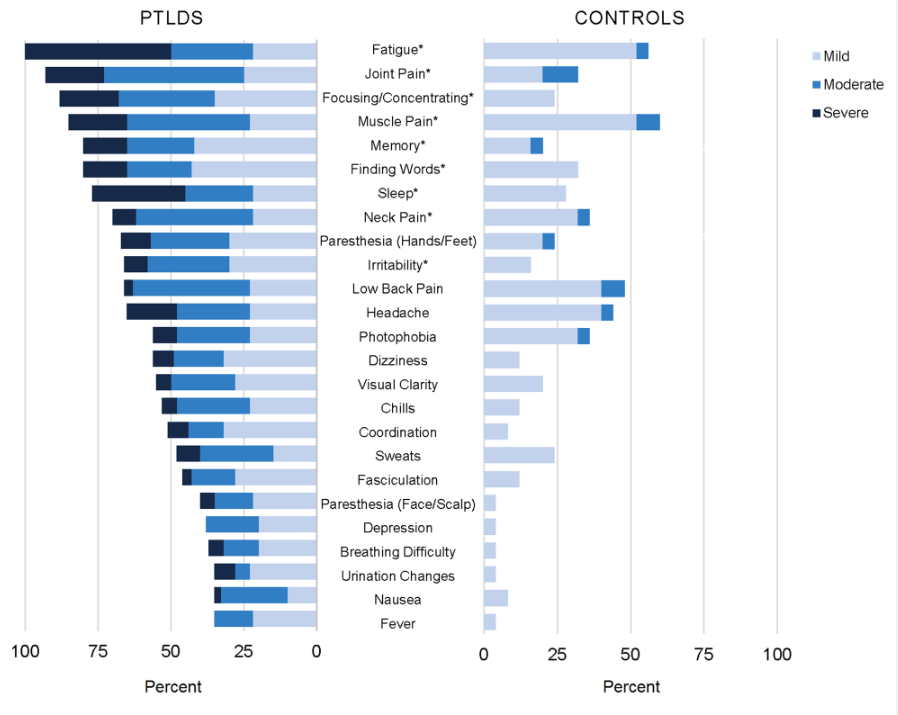
The chronic symptom burden related to Lyme disease is considerable, as shown on the left side of the graph above, and statistically significantly greater than the aches and pains of daily living experienced by the control group, on the right.
Risk factors for Post Treatment Lyme Disease include:
Increased severity of initial illness, the presence of neurologic symptoms, and initial misdiagnosis increase the risk of Post Treatment Lyme Disease. PTLD is especially common in people that have had neurologic involvement. The rates of Post Treatment Lyme Disease after neurologic involvement may be as high as 20% or even higher. Other risk factors being investigated are genetic predispositions and immunologic variables.
In addition to Borrelia burgdorferi, the bacteria that causes Lyme disease, there are several other tick-borne co-infections that may also contribute to more prolonged and complicated illness.
The causes of PTLD are not yet well understood but can be multifactorial. Our Center is investigating the potential roles of:
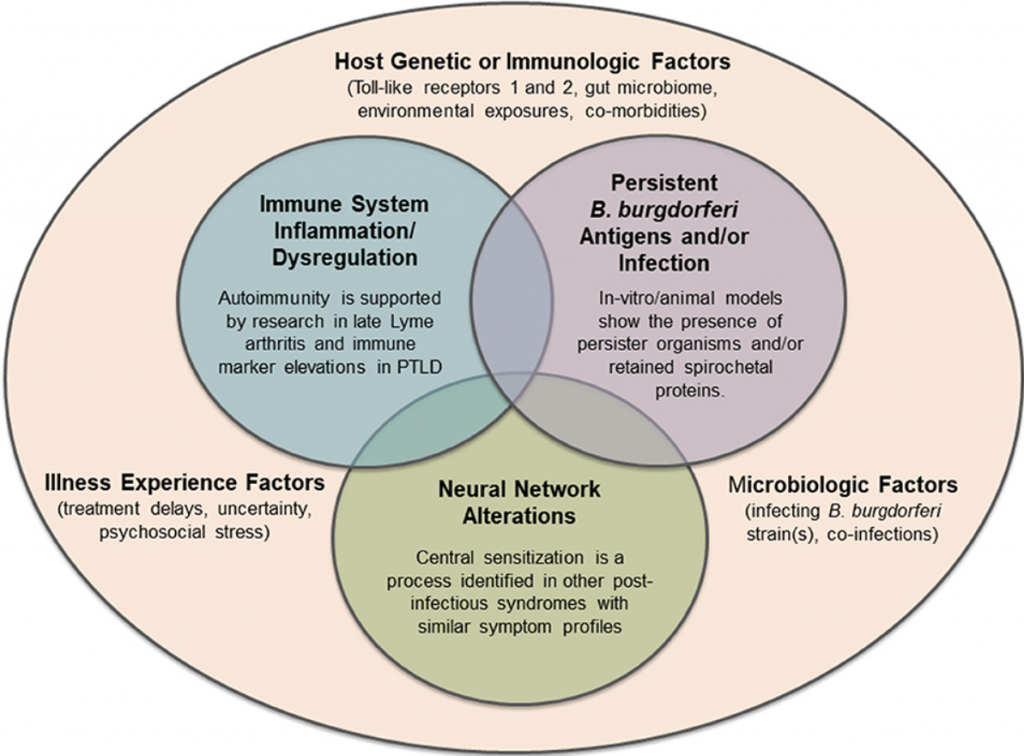
Our research has validated PTLD as a serious and impairing condition. However, the causes of PTLD are not yet well understood or validated, and the term PTLD does not mean post-infection or imply an assumption of underlying biologic mechanisms. The Lyme disease patient population is heterogeneous and the drivers of persistent illness can be varied and multifactorial. The roles of immune dysfunction, autoimmunity, chronic inflammation, persistent bacterial infection, persistent bacterial antigenic debris, neural network alteration, and other potential causative biologic mechanisms of PTLD are being investigated at our Center.
The persistent symptoms in Lyme disease can have a large negative impact on an individual’s health and quality of life. Patients often call this condition chronic Lyme disease, although an agreed upon clinical case definition for chronic Lyme disease has proven difficult to reach a consensus on.
PTLD is a narrow definition designed specifically to facilitate research and discovery. Research results can be extrapolated and generalized when appropriate to the much broader group of patients with chronic or persistent Lyme disease. In the clinical context there is an ongoing debate about renaming chronic Lyme disease to another name such as Long-haul Lyme, persistent Lyme disease, or Lyme disease associated chronic illness. However, the clinical name should not limit research into underlying causes and biomarkers for this persistent illness. The patient’s illness is real and the care of the patient remains paramount as we pursue multifactorial causes and a cure.
There are already an estimated 2 million patients in the US living with persistent or post treatment Lyme disease. With approximately 500,000 new U.S. cases of Lyme disease per year, the number of people experiencing chronic symptoms is a growing public health concern. Notably, many persisting Lyme disease symptoms overlap with other infection-associated chronic illnesses such as Long COVID and ME/CFS, and additional studies are needed to determine if they may share some common biologic pathways. Research at our Center aims to understand the biologic drivers of all manifestations of Lyme disease so that diagnostics can be improved, and more effective personalized treatments can be developed to enhance patients’ health outcomes.
Currently there are no FDA approved treatments for the persistent symptoms in Lyme disease. Therefore, treatments must be individualized by addressing specific findings, symptoms, and circumstances for each individual.
New treatment approaches are needed to address the long-term symptoms associated with Lyme disease which can be debilitating to patients and costly to society. In 2022, our Center began its first two treatment trials for patients with Lyme disease infection associated chronic illness. These pilot clinical trials are made possible thanks to the generous support of the Steven and Alexandra Cohen Foundation. More information about these trials can be found in our 2022 Impact Report.
Following antibiotic therapy, approximately 90% of late Lyme arthritis patients recover from extensive joint swelling, arthritis, and pain.
After extensive antibiotic treatment, approximately 10% of late Lyme arthritis patients remain symptomatic with a condition termed antibiotic refractory late Lyme arthritis. Extensive research has shown that the bacteria can no longer be found in the tissue or fluid of this subgroup of patients. However, recent research shows that peptidoglycans, from parts of Borrelia burgdorferi‘s cell wall, can remain behind in patients’ joints and trigger an immune reaction that could be perpetuating the inflammation observed in some Lyme arthritis patients.
Lyme disease encompasses a range of biologic processes and disease manifestations. Patients are often referred to the Lyme Disease Research Center for evaluation of chronic Lyme disease, an umbrella term that encompasses many heterogeneous subsets of illness. Examples of defined Lyme disease subsets include Post Treatment Lyme Disease (PTLD), and Antibiotic Refractory Late Lyme Arthritis. The mechanisms of these Lyme disease conditions are different and effective treatments need to be tailored accordingly.
Persistent symptoms of Lyme disease are similar to and overlap with other conditions involving fatigue, pain, and cognitive symptoms. Therefore, rigorous diagnostic evaluation is necessary to determine if Lyme disease could be the trigger for ongoing disease processes or if some other disease processes are involved.
Gaps in knowledge can lead to problems in clinical care. By distinguishing research subsets of Lyme disease, such as PTLD, our patient-centered clinical research program is illuminating the complex pathophysiology of the illness to improve diagnostics, treatments, and quality of life for patients.

Join our mailing list to receive the latest news and updates from Johns Hopkins Rheumatology and the Johns Hopkins Lyme Disease Research Center.